Tags
Aerosols, Close Talkers, Confined Space, Coronavirus, Covid-19, Dr. Christopher Gill, Droplets, Huggers, Humidity, HVAC, Indoor Transmission, Jacksonville, Outdoor Transmission, Public Health, SARS-CoV-2, Social Media, Time Magazine, Ultraviolet Light
I’m often inspired by social media because that’s where the sacred cows graze. Today I saw a juicy one… but actually, the linked article was not surprising: the headline claimed that Jacksonville, Florida residents were flocking to local beaches after they’d been reopened. What grabbed me were the half-witted condemnations made by the poster and his friends. One individual, a Jacksonville resident, claimed that the article was incorrect, that this was “not happening in Jax”. But many of the commenters were horrified by the accompanying photo, a view down the beach showing a number of walkers. If you’ve ever been to a beach, you probably know that such a visual perspective can exaggerate crowd conditions. They looked adequately distanced to me, and I’d bet most of the people or small groups in the photo were a good 20+ feet apart.
The comments on the post were a display of unbridled anger: those people on the beach would be sorry when they caused a second spike in coronavirus cases. How monstrous were these Jaxers to chance infecting others! A few expressed hope that the beachgoers would get sick, as if they’d learn their lesson. And in a delicious case of projection by the uninformed, the hashtag #FloridaMorons was trending on social media. These ugly, nitwitted nannies just can’t get over their need to control their fellow man, while lacking the knowledge to do so sensibly.
Not only did the people on the beach look adequately distanced to the rational eye, but unless you’re an unreformed hugger or “close talker”, the chance of contracting coronavirus outdoors is slim to none! That’s especially true on a beach, where there is typically a decent breeze.
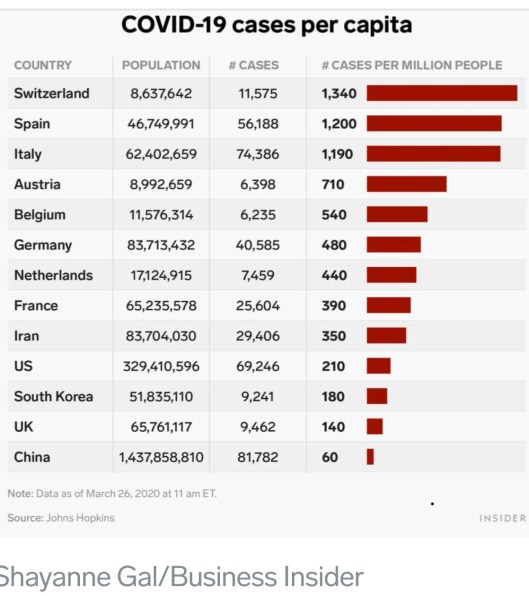
A recent study conducted by Chinese researchers on the environments in which clusters of Covid infections were originally contracted showed that outdoor transmission is very unlikely:
“…among our 7,324 identified cases in China with sufficient descriptions, only one outdoor outbreak involving two cases occurred.”
The authors conclude that coronavirus transmission is an indoor phenomenon.
A Q&A from Time includes the question: Is there any difference between being indoors and outdoors when it comes to transmission? Here is part of the response:
“We all occupy an area in three dimensional space, and as we move away from one another, the volume of air space on which we have an impact expands enormously. ‘If you go from a 10-ft. sphere to a 20-ft. sphere you dilute the concentration [of contaminated air] eight-fold,’ says Dr. Christopher Gill, associate professor of global health at Boston University School of Public Health.”
“‘Within seconds [a virus] can be blown away,’ […] Sunlight may also act as a sterilizer, Gill says. Ultraviolet wavelengths can be murder—literally—on bacteria and viruses, though there hasn’t yet been enough research to establish what exactly the impact of sun exposure is on SARS-CoV-2, the virus responsible for COVID-19.”
There is evidence, however, that high temperatures and humidity reduce the spread of the virus (and see here). That sounds like the beach to me! Whether by droplets or aerosols, confined spaces are where transmission happens. It is almost exclusively an indoors phenomenon, aggravated by HVAC air flows that create dry conditions.
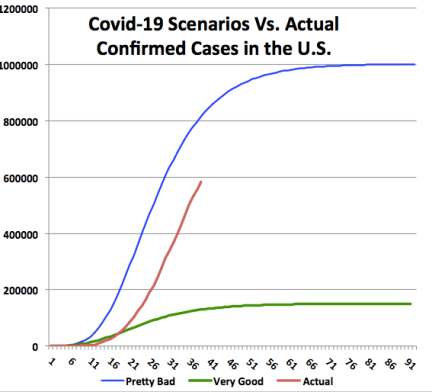
Social distancing is still important at the moment, but keeping people indoors is not conducive to public health. Most of the country (well, outside of downstate New York) is on a path to stanching the contagion. Under these circumstances, you can expect people to push back against unreasonable demands to stay off the beach, stay off an outdoor job, or even stay off their indoor job where there is good ventilation with fresh air, and where distance can be maintained. These little social-media tyrants should pry off their jack-boots and get some sand between their toes!