Tags
CARES Act, Covid-19, Don Wolt, Elective Procedures, HealthData.gov, HHS, Hospital Layoffs, Hospital Utilization, ICU Occupancy, Influenza Admissions, Inpatient Occupancy, KPI Institute, Observational Beds, Optimal Utilization, PPE Shortfalls, Seasonal Occupancy, Staffed Beds

Here’s one of the many entertaining videos made by people who want to convince you that hospitals are overrun with COVID patients (and here is another, and here, here, and here). That assertion has been made repeatedly since early in the pandemic, but as I’ve made clear on at least two occasions, the overall system has plenty of capacity. There are certainly a few hospitals at or very near capacity, but diverting patients is a long-standing practice, and other hospitals have spare capacity to handle those patients in every state. Those with short memories would do well to remember 2018 before claiming that this winter is unique in terms of available hospital beds.
An old friend with long experience as a hospital administrator claimed that I didn’t account for staffing shortfalls in my earlier posts on this topic, but in fact the statistics I presented were all based on staffed inpatient or ICU beds. Apparently, he didn’t read those posts too carefully. Moreover, it’s curious that a hospital administrator would complain so bitterly of staffing shortfalls in the wake of widespread hospital layoffs in the spring. And it’s curious that so many layoffs would accompany huge bailouts of hospital systems by the federal government, courtesy of the CARES Act.
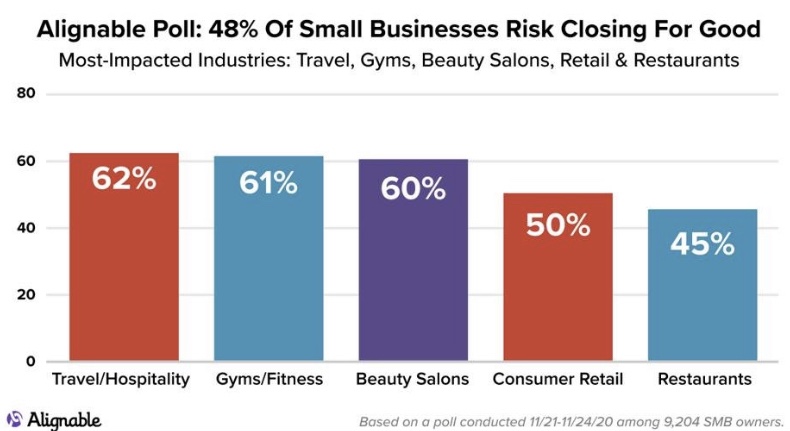
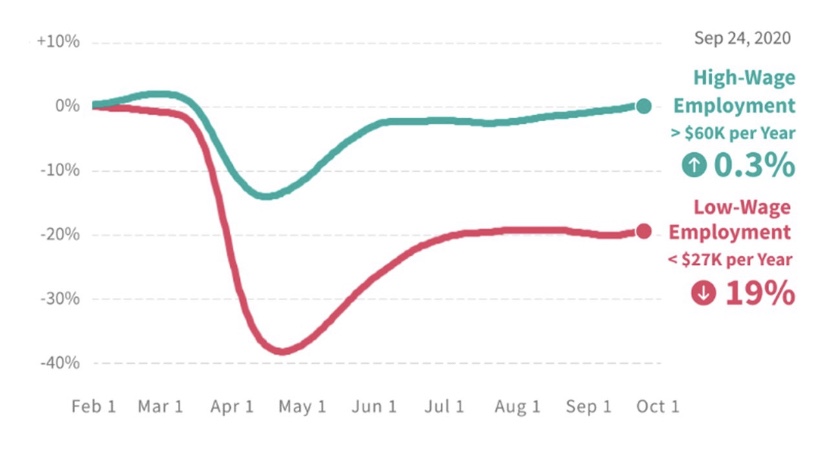
In fairness, hospitals suffered huge declines in revenue in the spring of 2020 as elective procedures were cancelled and non-COVID patients stayed away in droves. Then hospitals faced the expense of covering their shortfalls in PPE. We know staffing was undercut when health care workers were diagnosed with COVID, but in an effort to stem the red ink, hospitals began laying-off staff anyway just as the the COVID crisis peaked in the spring. About 160,000 staffers were laid off in April and May, though more than half of those losses had been recovered as of December.

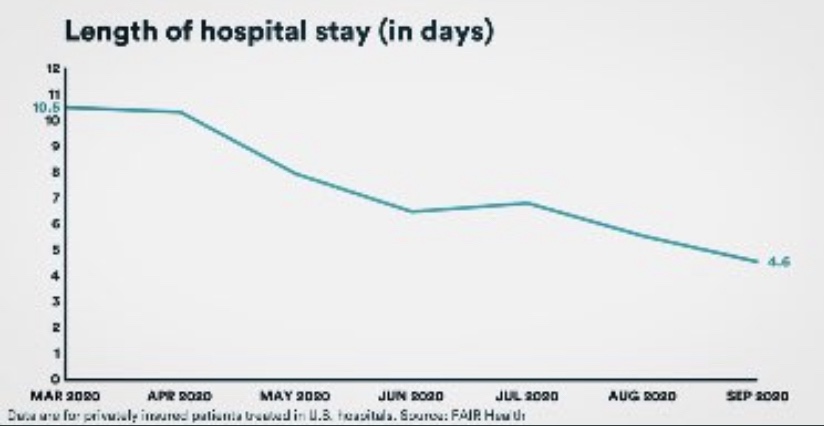
Did these layoffs lead to a noticeable shortfall in hospital capacity? It’s hard to say because bed capacity is a squishy metric. When patients are discharged, staffed beds can ratchet down because beds might be taken “off-line”. When patients are admitted, beds can be brought back on-line. ICU capacity is flexible as well, as parts of other units can be quickly modified for patients requiring intensive care. And patient ratios can be adjusted to accommodate layoffs or an influx of admissions. Since early in the fall, occupancy has been overstated for several reasons, including a new requirement that beds in use for observation of outpatients with COVID symptoms for 8 hours or more must be reported as beds occupied. However, there are hospitals claiming that COVID is stressing capacity limits, but nary a mention of the earlier layoffs.
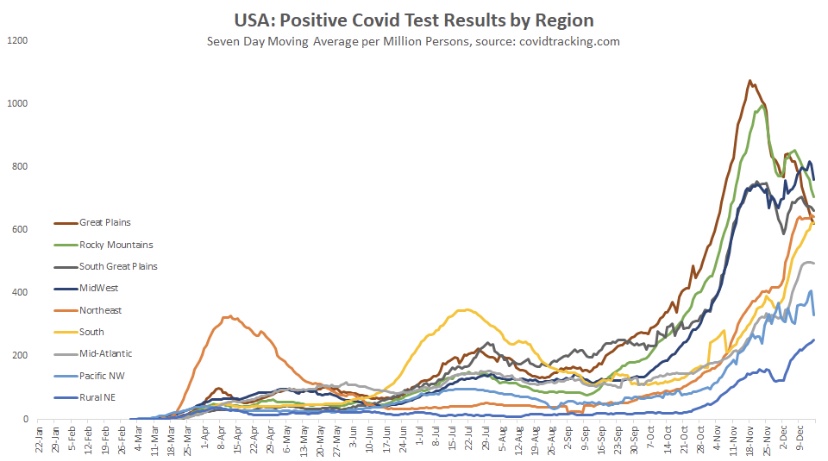
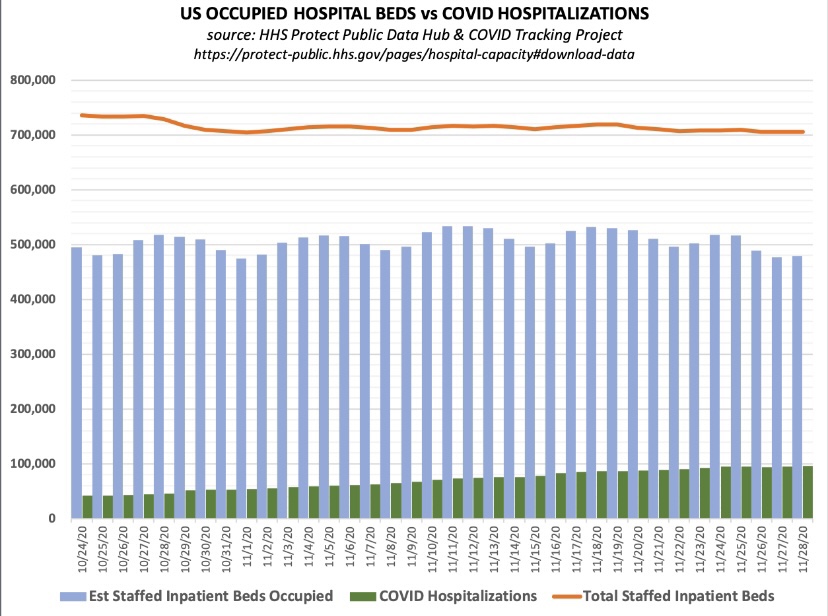
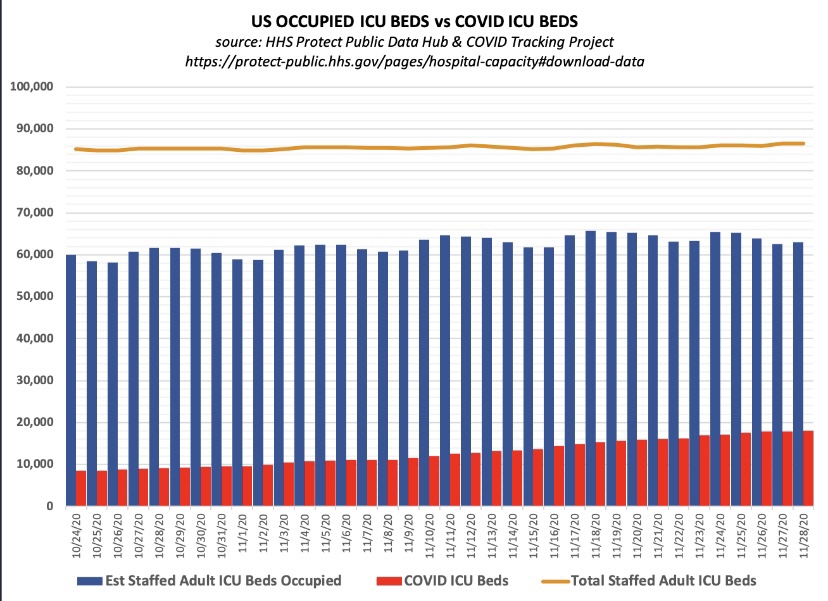
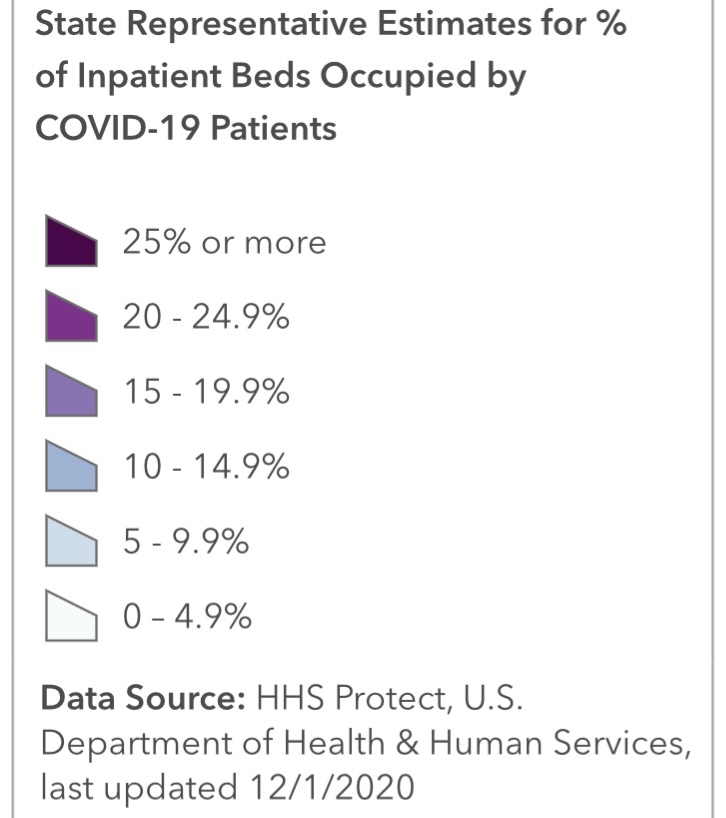
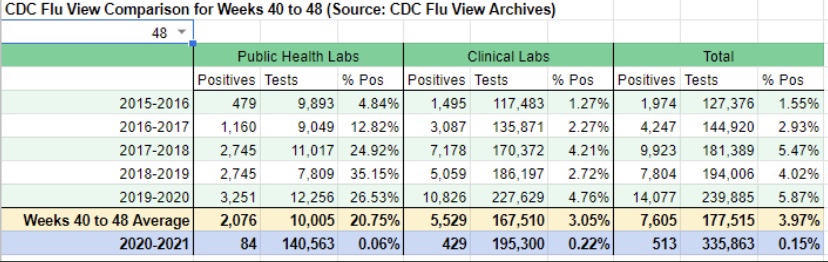
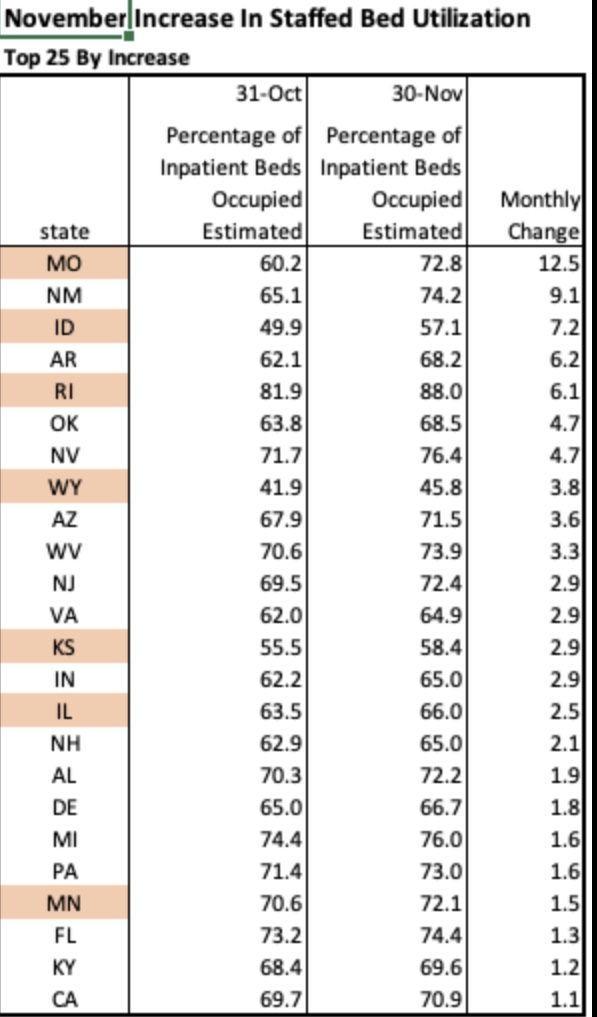
So where are we now in terms of staffed hospital occupancy. The screen shot below is from the HHS website and represents staffed bed utilization nationwide. 29% of capacity is open, hardly a seasonal anomaly, and there are very few influenza admissions thus far this winter, which is rather unique. 37% of ICU beds are available, and COVID patients, those admitted either “for” or “with” COVID, account for less than 18% of inpatients, though again, that includes observational beds.

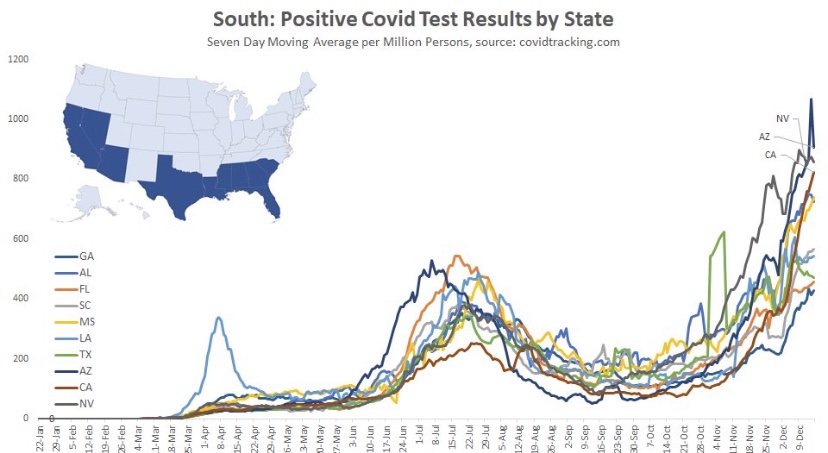
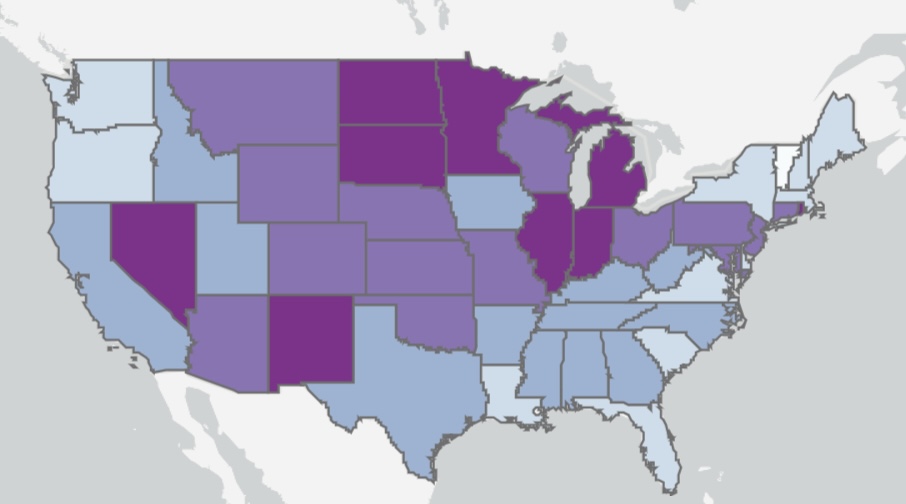
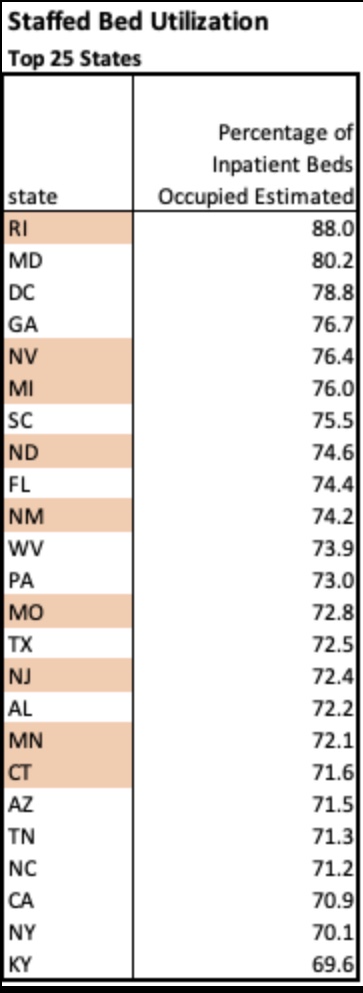
Next are the 25 states with the highest inpatient bed utilization as of January 7th. Rhode Island tops the list at just over 90%, and eight other states are over 80%. In terms of ICU utilization, Georgia and Alabama are very tight. California and Arizona are outliers with respect to proportions of COVID inpatients, 41% and 38%, respectively. Finally, CA, GA, AL and AZ are all near or above 50% of ICU beds occupied by COVID patients.

So some of the states reaching the peak of their fall waves are pretty tight, and there are states with large numbers of very serious cases. Nevertheless, in all states there is variation across local hospitals to serve in relief, and it is not unusual for hospitals to suffer wintertime strains on capacity.
Los Angeles County is receiving much attention for recent COViD stress placed on hospital capacity. But it is hard to square that narrative with certain statistics. For example, Don Wolt notes that the state of California reports available ICU capacity in Southern CA of zero, but LA County has reported 10% ~ 11% for weeks. And the following chart shows that LA County occupancy remains well below it’s July peak, especially after a recent downward revision from the higher level shown by the blue dashed line.

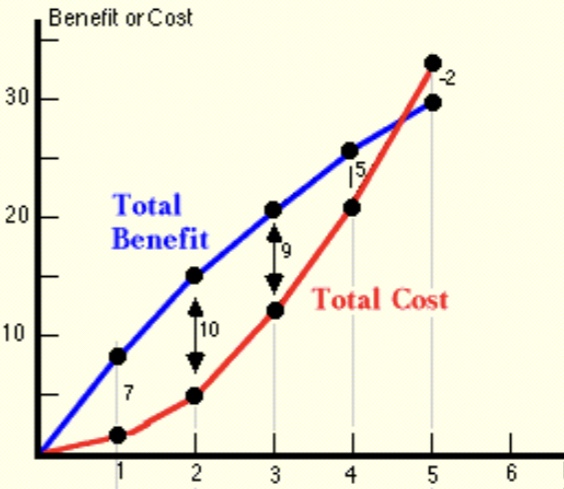
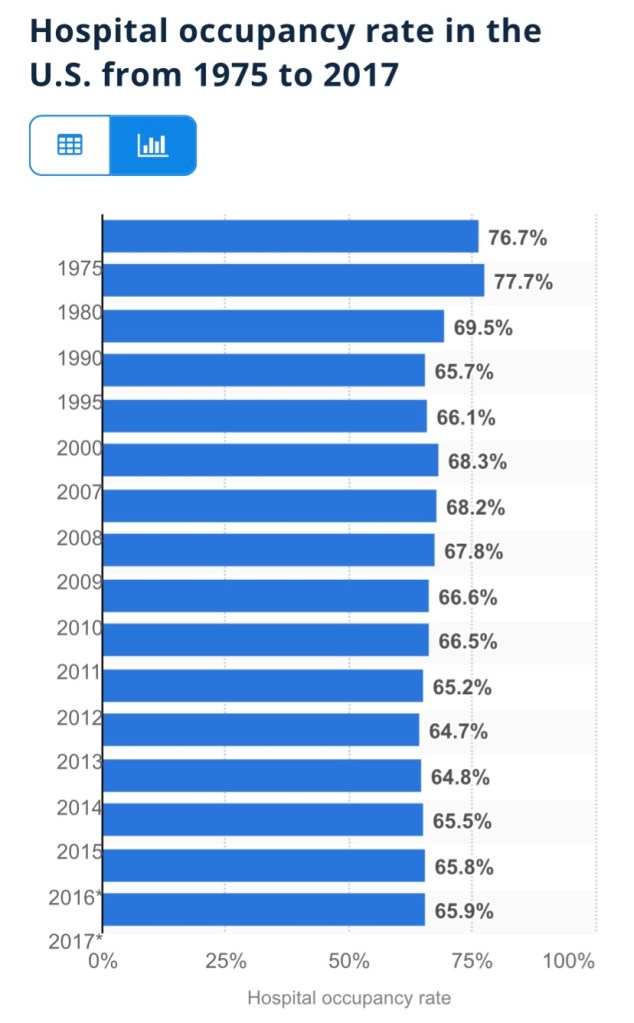
Interestingly, the friend I mentioned said I should talk with some health system CEOs about recent occupancies. He overlooked the fact that I quoted or linked to comments from some system CEOs in my earlier posts (linked above). It’s noteworthy that one of those CEOs, and this report from the KPI Institute, propose that an occupancy rate of 85% is optimal. This medical director prefers a 75% – 85% rate, depending on day of week. These authors write that there is no one “optimal” occupancy rate, but they seem to lean toward rates below 85%. This paper reports a literature search indicating ICU occupancy of 70% -75% is optimal, while noting a variety of conditions may dictate otherwise. Seasonal effects on occupancy are of course very important. In general, we can conclude that hospital utilization in most states is well within acceptable if not “optimal” levels, especially in the context of normal seasonal conditions. However, there are a few states in which some hospitals are facing tight capacity, both in total staffed beds and in their ICUs.
None of this is to minimize the challenges faced by administrators in managing hospital resources. No real crisis in hospital capacity exists currently, though hospital finances are certainly under stress. Yes, hospitals collect greater reimbursements on COVID patients via the CARES Act, but COVID patients carry high costs of care. Also, hospitals have faced steep declines in revenue from the fall-off in other care, high costs in terms of PPE, specialized equipment and medications, and probably high temporary staffing costs in light of earlier layoffs and short-term losses of staff to COVID infections. The obvious salve for many of these difficulties is cash, and the most promising source is public funding. So it’s unsurprising that executives are inclined to cry wolf about a capacity crisis. It’s a simple story and more appealing than pleading for cash, and it’s a scare story that media are eager to push.